The robots, multilimbed and wielding nimble metal fingers, are intricate and imposing. One, the intuitive da Vinci robot, towers over the surgical table, its four hands ready to twist and tilt. The other, the more petite and pliable Medrobotics Flex robot, is capable of navigating to places in the body previously unreachable by the human hand. Both are the new standard of care, and yet each is subject to surgeons, the masters at the controls.
“Robotics are a tool … that if used right, could augment the ability of surgeons to perform more complex surgery,” explains Gaby Moawad, MD, RESD ’11, associate professor of obstetrics and gynecology at the George Washington University (GW) School of Medicine and Health Sciences (SMHS). “[It] is like you have a calculator. There are lots of people who can do math really quickly, but using the calculator would enhance your ability to do calculus quicker. That’s robotic surgery.” At GW Hospital, robotic surgery and its partner, minimally invasive surgery, are enabling the institution to swiftly move ahead of trend: The hospital has performed 3,000 robotic surgeries, the most in the region, and it was the first to have the Medrobotics Flex robot and use it for colorectal surgeries.

Robot vs. Robot
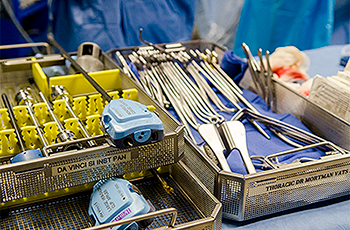
Although it’s easy to become enamored with the idea of robots, Vincent Obias, MD, chief of the Division of Colon and Rectal Surgery and associate professor of surgery at SMHS, is quick to point out that they are merely an extension of the surgeon. The da Vinci robot, the go-to for abdominal, colorectal, thoracic, and gynecologic surgeries, requires the surgeon to sit in a console and control each of the four arms using fingers, hands, and feet. Take an abdominal surgery: First, Obias makes a small incision to insufflate, or distend, the abdomen so there’s space to work; then, he makes additional small incisions to put in place the trocars, or sharp-tipped pins with a hollow tube and a seal through which instruments are inserted; once those are secure and the patient is in position, Obias docks the robot. “We can [then] break scrub and walk a few feet away to where the console is, [where we] control the robot,” he says. There, Obias has the advantage of 3D stereoscopic vision, which allows for better visualization, and each arm has tremor control, ensuring improved precision, critical for surgeries in which millimeters matter and meticulousness is paramount. The robot also boasts what thoracic surgeon Keith Mortman, MD, associate professor of surgery at SMHS, calls “seven degrees of freedom.” “We can essentially rotate 360 [degrees]; I haven’t figured out a way to actually rotate my wrist 360 degrees,” he says. “So the robotic instruments can move in ways that the human wrist can’t, and when you’re working in a very tight space, that’s really where the utility of the robot comes into play.” And when it comes to tight spaces, the Medrobotics Flex robot, commonly used for head and neck and colorectal surgeries, is in its element. “Instead of having a rigid camera that we place through the mouth, it’s a flexible camera that allows us to get into different areas that we wouldn’t have been able to before,” says Arjun Joshi, MD, associate professor of surgery. Because of that improved access, Joshi, a head and neck surgeon, can better treat certain diseases. Previously, while removing tumors on the tonsils or at the base of the tongue, he would have to split the jaw. He also is now better able to treat certain types of cancer, as the robot makes access to hard-to-reach tumors easier.
Practice Makes Perfect

As with most other tools, however, using the robot requires training and practice. Most secondary training includes a fellowship, simulations, cadaver dissections, and proctored cases until surgeons are credentialed to perform robotic surgeries solo. Once a surgeon has mastered the robots, it’s essential, Moawad says, to keep training and maintaining skills. “If you ran a marathon last year, you can’t just sign up and say, ‘Tomorrow I’m running a marathon because I ran it last year.’ You need to train for it,” he says. “So training is very important, and the maintenance of skills is very important. If you don’t do it very frequently, you’re not going to be as efficient; you’re not going to maintain your mastership level that you acquired during training.”
It’s the Little Incisions That Count
Although many surgeons subscribe to the wonders of robotic techniques — including the youngest generation just entering the field — minimally invasive surgery (MIS) is equally important in the world of advanced surgical methods. Minimally invasive surgery is the parent of robotic surgery, or, as Obias explains, “robotics is minimally invasive surgery, but not all minimally invasive surgery is robotics.” In other words, depending on the procedure and the surgeon’s assessment, minimally invasive procedures performed by hand could be better or more appropriate than those done using the robot. “MIS, or minimally invasive approaches for any kind of surgery, is now mainstream,” says Khashayar Vaziri, MD, associate professor of surgery at SMHS. “The more complex operations still take some more advanced training, but the majority of routine operations performed in any field, whether it’s general surgery, vascular surgery, thoracic surgery, [or] colorectal surgery … are almost all being performed in a minimally invasive fashion.” At GW Hospital, he adds, the majority of complex operations, such as gastrectomies for cancer, complex hernia repairs, and bariatric surgeries, are done minimally invasively. The field itself is also witness to advancements, in addition to robots. “Now we also have advanced tools, advanced sealing devices, advanced staplers,” Vaziri says. “All of these advances in surgical instruments and visualization are geared toward the minimally invasive realm.”

What’s key to MIS as a whole, including robotic surgery, is minimizing the need for large incisions. In thoracic surgery, for example, incisions in the chest are more painful than elsewhere on the body because the chest wall has more nerve fibers. “So we know that the small incisions hurt less, and there’s plenty of data now that show the amount of [pain medication] patients need afterward is less, both subjectively and objectively,” Mortman says. Additionally, with chest surgeries, smaller incisions heal faster, which means surgeons can remove drainage tubes faster, and hospital stays are therefore shorter — and that’s where the true value of minimally invasive procedures lies: with the patient. “Being able to [perform surgery] through the little incisions with these advanced technologies is better for the patient because many times, the visualization is better for the surgeon,” Vaziri explains. “The patients will have less pain, they’ll be hospitalized for a shorter period of time, their overall recovery will be shorter, and their return to a normal life and work will be faster without compromising the integrity of the operation.” No one, he adds, wants to have an operation, so the less traumatic the physicians can make surgical intervention, the better.
What Lies Ahead
As minimally invasive and robotic surgeries become the method of choice for most surgeons, particularly those at GW Hospital, the question remains: What will these techniques look like in the future? Right now, the da Vinci robot and the Medrobotics Flex robot are the most readily available tools on the market. But the field is rapidly expanding as new companies enter the robot market, such as Google and Johnson & Johnson. Enhanced visualization is also a new target for surgeons. GW Hospital, for example, is currently home to Precision VR, a 3D virtual reality tool primarily used by neurosurgeons to plan surgical pathways with patients’ specific pathologies. Mortman, however, has incorporated the technology into thoracic surgeries, which has inspired potential new visual tools. “Is there a way to [take] the virtual reality images that we use and then overlay them with the robotic cases?” Mortman asks. “Can we actually pull up the VR images into the robot, so if there’s a question, as we’re actually doing the operation with the robot, about the anatomy — how big is the mass, what’s the relationship with the mass to this major blood vessel — can we overlay the virtual reality images to help us out in real time?” It’s an idea that has also occurred to Moawad, who is developing a way to include augmented reality in his surgeries. He asks, “For example, what is the length of incision that you need to do? How deep should you go to find the pathology? What are the margins of excisions that are safer? That’s the role of augmented reality and artificial intelligence, to make surgery simplified.” Regardless of method, it’s clear that robotic and minimally invasive surgeries aren’t just the future; they’re also the present — and they inspire passion in the surgeons who perform them. “I love it,” says Obias. “I love being on the cutting edge.”